Continuum Long Term Survivor Study (CLTSS)
Summary of Project
A great deal of progress has been made in our understanding of the basic biology of common cancers. This has led to rapid development of new targeted drugs and immune therapies, which have been hugely beneficial for many patients.
Some cancers are amenable to long term treatment with single or sequential drug therapies. However, in these patients there is often a persistent small amount of cancer in the body as shown by CT or MRI scans. In other words modern cancer treatments reduce the volume of cancer and hold the remainder ‘in check’, and this results in excellent cancer control and quality of life, but the cancer usually progresses eventually.
A rare set of patients respond completely to their cancer treatment, and are able to live tumour free for greater than 5 years. This study aims to examine these long term survivors of cancer who are completely disease free. The biological basis of this excellent outcome is not understood, and although immune mechanisms are suggested there is no definitive evidence to date to show how this may actually occur. If we can understand the underlying mechanisms behind these rare durable disease-free outcomes in these fortunate individuals, we may be able to design new treatments for patients who are not responding.
This study is funded by Continuum Life Sciences.
Scientific background of the study
Recent advances have allowed detailed evaluation of a patient’s general immune function. Scientists believe that certain patients have proteins on their tumour surface which show strong similarity to viral or bacterial proteins, and this has a positive impact on their long term outcome and survival. In other words, in these patients, the cancer was possibly being regarded as an infection by the immune system and, as such, rapidly and efficiently ‘rejected’. We aim to look for this form of recognition and tumour rejection in the stored tumour tissue of long term cancer survivors, taken prior to treatment, and who went on to have complete elimination of their cancer, despite having a high disease burden initially. Further understanding and corroboration of this process would quickly influence new immune-based treatments for other patients.
Scientific background of the study – In detail
Recent technological advances have allowed detailed evaluation of the tumour microenvironment (TME), outlined key mechanisms of immune suppression and allowed design of new immunotherapy strategies. One key element in the TME is the tumour itself where mutations lead to generation and expression of new proteins on the tumour surface, so called neoantigens. These neoantigens are recognised by infiltrating T cells which are either allowed to fulfil their toxic function and kill tumour cells, or are subdued by other immune cells by the expression of immune-inhibitory mechanisms. Recent studies have indicated that tumours with the highest neoantigen number combined (and not independently) with the densest cytotoxic T cell infiltrate inside the tumour predicted long term survival in pancreatic cancer (PDAC). Furthermore it has also been shown that patients whose neoantigens show strong similarity to viral or bacterial proteins, so called molecular mimicry, had a positive impact on their long term outcome and survival. Corroboration of this form of molecular mimicry in the archival tumour tissue of long term survivors across a number of aggressive cancers is one way in which analysis of the TME of such patients could lead to new interventional approaches using microbial proteins to induce such immunity before/after surgery with high potential impact on patient survival.
In addition, there is emerging evidence that certain microbes (bacteria) in our gut may have a significant effect on the function and efficiency of our immune system and may contribute to the long term disease free outcomes in cancer patients. The microbial make-up in the bowel is called the ‘microbiome’ and comprises a large array of bacterial species, the interplay between which may directly influence the way the immune system responds to evolving cancers and may help tumour rejection/destruction.
We will compare long term survivors with control participants who will be healthy volunteers and also current cancer patients who we hypothesise won’t have proteins which mimic bacterial/viral proteins on the surface of their tumours (healthy volunteers will only have their blood and stool analysed) and will have different gut flora to long term survivors.
Therefore a full evaluation of immune function in these long term survivor patients and control participants will include blood-resident immune cells, HLA tissue typing (Identifying which type of HLA proteins are present on their tissue – these proteins are responsible for regulating the immune system), an examination of their complete medical history and concurrent diseases, examination of their original cancer tissue (which will be stored in an archive in paraffin wax) and an insight into the bacterial populations in the gut which can be determined using stool samples.
WOULD YOU LIKE TO GET INVOLVED?
We are searching for long term survivors of cancer. In order to be eligible for the study you must answer ‘yes’ to all of the following Inclusion criteria:
Inclusion criteria:
• Are you a long term survivor (having been clear of cancer for 5 years OR have been living with cancer for more than 5 years) of an aggressive, locally advanced and/or metastatic cancer (cancer that has spread beyond the organ of origin which was treated with surgery, immuno, chemo or radiotherapy.
• Will you allow access to and use of medical history and personal data?
• Are you willing to complete a lifestyle questionnaire?
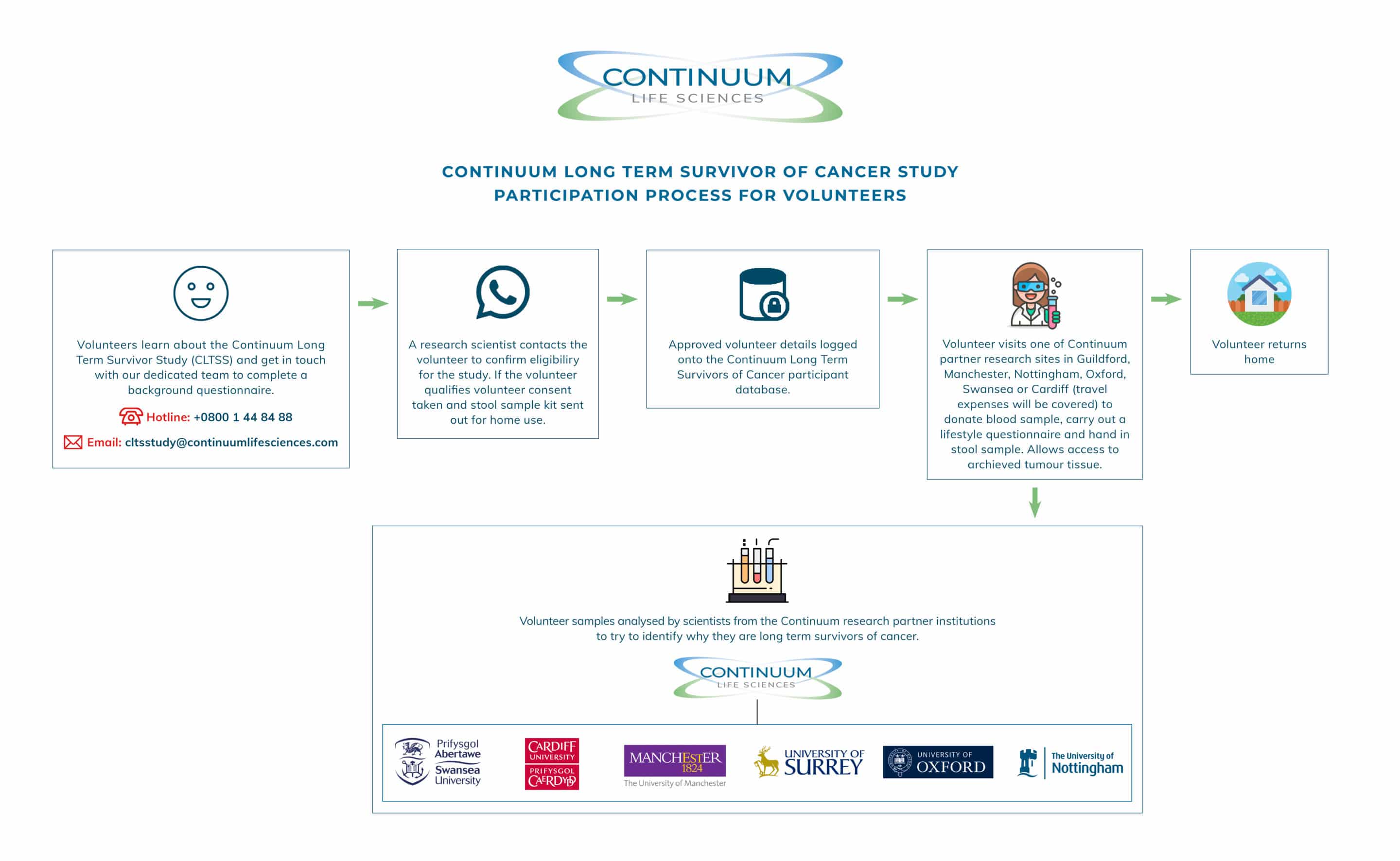
• Are you willing/able to travel to one of our blood donor centres (you will receive travel expenses) to donate blood (50mls)?
• Are you willing/able to donate a stool/poo sample (you will be given a kit to do at home and asked to return it in the post)?
• Will you allow access to your stored tumour tissue?
• You have received no cancer treatment for greater than 5 years and had no visible cancer on any of your scans for greater than 5 years?
OR
• Have you been living with cancer for over 5 years and receiving treatment.
If you or anyone you know fit all of the inclusion criteria for the study and are interested in taking part. Please contact us using the following:
email us at cltsstudy@continuumlifesciences.com
or alternatively call +0800 1 44 84 88
“At Surrey University we are very excited and inspired by this project. The long-term survivor study and collaboration with Continuum may be one of the most important studies for decades. The focus on a large cohort of carefully defined individuals ‘cured’ of their cancer, combined with state-of-the-art technology to determine the basis of the immune cell recognition of their cancer will underpin the ultimate aim. This is to create new immunotherapy drugs to replicate the same mechanisms observed in these cured patients. We anticipate 2 outcomes: a bespoke personalised treatment, based on reprogramming an individuals T cells in the test tube and giving them back again, and an on-the-shelf vaccine for any patient, given repeatedly over months, to re-direct the immune system against cancer cells.”> and giving them back again, and an on-the-shelf vaccine for any patient, given repeatedly over months, to re-direct the immune system against cancer cells.”
Professor Hardev Pandha
Professor of Medical Oncology, University of Surrey